When I design a plan of supplementation for my clients, always base my recommendations on a thorough assessment of your nutritional status and biochemical, using a blood test as a reference. However, there are three supplements that I recommend almost without exception. Over the next three articles in my blog, I would like to delve into each of these supplements essential: vitamin D (especially in winter), the omega-3 and glycine. Let’s start with the first: the vitamin D.
Introduction. What vitamin or a hormone?
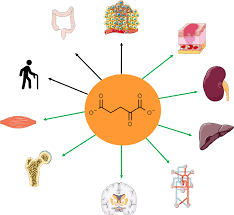
All nutrients are important: the need to fulfill essential functions in the body. However, if I had to choose one for their relevance, it would be vitamin D. No other nutrient performs so many important functions and various, or affects so many different systems of the body. Although commonly called a vitamin, in reality , it is more accurate to consider it a hormone. This is because it is not necessary to eat it, because the body can produce it on the skin when exposed to the sun. Once produced, it travels through the bloodstream, it is transformed into different organs (like the liver and kidneys) and it acts on various body systems, including the musculoskeletal, immune, cardiovascular, and neuronal.
Cycle
This is the cycle of the vitamin D3 that we get mainly from the sun, its most important source, as we will see later:
- Skin: the outer most layer of skin (epidermis), we have a molecule called 7-dehydrocholesterol, which acts as a provitamin D3′. Interestingly, it is also a precursor of cholesterol in the blood. When the ultraviolet rays (UV-B) from the sun come in contact with this molecule, is converted into vitamin D3 (cholecalciferol), which travels through the blood to the liver.
- Liver: once in the liver, the enzyme CYP2R1 transformed the D3 25-hydroxy (OH) D3, also known as calcidiol. This is an inactive form of the vitamin, a pro-hormone that is measured in the laboratory analyses of blood.
- Kidney: In the kidneys, the calcidiol is converted into 1,25-dihydroxy (OH2) D3, or calcitriol, the active form of vitamin D. calcitriol is the hormone responsible for performing the crucial functions that we will discuss later.
- Bile – Gut: The enzyme CYP24A1 degrades excess calcitriol, transforming it into 1,24,25-dihydroxy (OH3) D3, or acid calcitroico, a metabolite inactive, are excreted through the bile, and excreted in the intestine.
The vitamin D that we get from food (D2) follows the same cycle that the D3 from the sun once it reaches the liver through the digestive system.
Types
According to the cycle described above, and these are the main types of vitamin D:
- Cholecalciferol (D3)is Produced naturally in the skin when exposed to sunlight. It is also found in foods of animal origin such as cod liver oil, egg yolk and oily fish. It is the most common form of supplementation.
- Ergocalciferol (D2): it Comes from plants, particularly fungi and yeasts. Unlike cholecalciferol, is not obtained from the sun. Although it can be taken as a supplement, it is less effective to increase the levels of vitamin D compared with the D3.
- Calcidiol: storage Form of vitamin D3 in the body, produced in the liver from cholecalciferol. It is stored in fatty tissues and is inactive (prohormone). Calcidiol levels in blood are used to measure the amount of vitamin D in the body. Sometimes we use the term ‘calcifediol,’ which is the form used as a drug (Hidroferol) in the Spanish Social Security to correct deficits, although it is not the ideal way to supplement, except in specific cases that will be detailed later.
- Calcitriol: The active form of vitamin D produced in the kidney from calcidiol. It functions as a steroid hormone.
- Acid calcitroico: Metabolite inactive calcitriol, excreted in the bile to regulate the excess of vitamin D.
Features and Benefits for the Health
Vitamin D is primarily known for its role in bone health by facilitating the uptake, fixation and regulation of calcium and phosphorus in the bones and teeth, which becomes a key factor to prevent osteoporosis and osteomalacia. However, its scope goes far beyond this. Vitamin D regulates the expression of over 1,000 genes (study), and participates in various physiological functions, key, such as:
- Growth and cell death (apoptosis): Controls these processes essential for cell renewal.
- Angiogenesis: Promotes the formation of new blood vessels.
- Immune system: Modulates the immune system and the inflammatory response.
- Prevention of cancer: Decreases the risk of cancer of the breast, colon and prostate.
- Regulation of autoimmune diseases: Reduces the risk of diseases such as type 1 diabetes, rheumatoid arthritis, multiple sclerosis and depression.
- Glucose metabolism: Increases insulin sensitivity and regulates its secretion in the pancreas.
- Muscle and joint pain: Helps to reduce the pain in the muscles, joints and bones.
- Neurological development: Aid to the development of the brain and the nervous system.
Here are some studies that underscore the importance of maintaining optimal levels of vitamin D in relation to various diseases.
Relationship with Disease
Immune system. Infectious diseases, and autoimmune
Vitamin D plays a key role in the immune system, since its receptors are present on various immune cells, such as B cells, T and antigen-presenting. This allows you to regulate both immune responses innate (immediate and non-specific against infections) and adaptive (production of specific antibodies against pathogens) (study).
- Autoimmune diseases: vitamin D deficiency increases the risk of developing autoimmune diseases such as multiple sclerosis, rheumatoid arthritis, type 1 diabetes, lupus, and autoimmune hypothyroidism, among others.
- Infections: low Levels of vitamin D also make people more susceptible to viral and bacterial infections.
A meta-analysis that examined the relationship between vitamin D levels and mortality for COVID-19 concluded the following: ‘it suggests a theoretical point of mortality to zero at levels of approximately 50 ng/mL of vitamin D3 in the blood‘. This raises the question: how many lives could have been saved, and how many millions of euros in health costs could have been avoided if they would have supplemented the population to keep those optimal levels of vitamin D, whereas a bottle of vitamin D costs around € 20 and can last up to three years?
Alzheimer’s disease
A recent study from march 2023 followed more than 12,300 people over for 10 years, assessing the incidence of dementia among those who suplementaban with vitamin D and those that did not. The results revealed that proper supplementation was associated with a 40% lower risk of developing dementia. This effect was even more pronounced in people without a genetic predisposition to Alzheimer’s (that is to say, without the gene variant APOE4), where the risk was reduced to 47%.
Cancer
Numerous studies demonstrate an association between adequate levels of vitamin D and a reduced risk of developing cancer, as well as a better survival once the disease has manifested. This is explained by the role of vitamin D in the regulation of the immune system, the formation of new blood vessels (angiogenesis) and the control of growth and cell death (apoptosis). A study recently showed a significant reduction in cases of advanced cancers (metastatic and fatal) in people who are suplementaban with vitamin D and Omega-3 in comparison with those that did not. The risk reduction was even more noticeable in people without overweight.
Depression, schizophrenia and mental health
To achieve adequate levels of vitamin D may have a positive impact on the mental health and well-being of the brain. Although the precise mechanisms are still not fully understood, it is suggested that the decrease inflammation, increase cognitive function, neuronal protection, and the modulation of the neurotransmitters are involved.
A Finnish study observed that supplementation with vitamin D during pregnancy and childhood, reduced the risk of developing schizophrenia in adulthood. In addition, it has been found an association between low levels of vitamin D and an increase in depression, mood symptoms (pms) in women, and cognitive impairment in older persons (study).
Two clinical trials reinforce these findings:
- Seasonal affective disorder: A study compared phototherapy with the supplementation of vitamin D and found that both methods were beneficial in improving the symptoms in only one month (study).
- People with overweight and obesity: This assay revealed that individuals with low levels of vitamin D were more likely to suffer depression. Supplementation for a year led to a significant improvement in symptoms of depression (study).
Aging
The telomeres are structures at the ends of chromosomes whose main function is to protect the DNA in our genetic material. If you imagine a chromosome as a shoelace, the telomeres would be the diamond studs (the ends of plastic that protect the cord). Each time a cell divides to regenerate tissue or to repair damage, which occurs billions of times a day, the telomeres are shortened. Over time, as we age, these telomeres become shorter and shorter, which makes the DNA more exposed and increases the risk of genetic defects, accumulation of genome damage, and aging-related disease.
According to a study, higher levels of vitamin D through supplements can reduce the telomere shortening due to mechanisms of anti-inflammatory and anti-proliferative, suggesting that this vitamin may play a protective role in the aging process.
Hypertension
A study showed that supplementation with vitamin D during the winter months (when the sun exposure is less) reduced the systolic pressure, especially in those who took the highest dose of 4,000 IU/day, decreasing the pressure on -4,0 mm Hg. In addition, for each increase of 1 ng/ml in the vitamin D levels in the blood, we observed a reduction of 0.2 mm Hg in the systolic pressure.
Asthma
In patients with deficiency (<30 ng/ml) vitamin D supplementation reduced the rate of duration of asthma in a 27%, and improved lung function (study).
Here is the second part.