In my clinical practice, it is very common to reach a person with the results of an analytical and tell me: ‘I have everything well, well… except for the cholesterol.’ And then, when I check the results, they are surprised when I tell them: ‘Well… actually, there are many things that are correct, except cholesterol, which got it right.’ That is to say, both the people and many doctors remain calm when a biomarker in the results sheet of your analytics does not ‘bring an asterisk’ or not, ‘comes out in bold’, that is to say, when it is not out of the rank ‘officer’.
Ranges “official”
Although I have already addressed this issue in my books earlier, by the widespread confusion that exists, and by the importance that it has, I want to explain again why I don’t do (much) case to the ranks of “officers” (which appear on the leaves of the analysis), and management, other: ranks “optimal”. There are two main reasons.
First. The ranges of ‘officers’ in the leaves of the analysis are calculated based on a standard deviation, that is to say, establishes a range above and below the mean of the values that people “sound’ of a population. But this calculation is not always the right one. For example, if in a population, there is a generalized deficit (as is usually the case of vitamin D) or too wide (as can occur with glucose, insulin, triglycerides, homocysteine, etc), these ranges are poorly established because they are based on inaccurate information.
Second. Even if the rank ‘officer’ is not affected by the above, and is well calculated, that something is just above or below these thresholds only means that there is a deficit or a surplus, but that is not the same as saying that the level is ‘optimal’. These ranges officers are very broad and that something is within range does not mean that it is at its best level. The body does not work the same when it simply has no deficit when a biomarker is in its ‘best site’. In addition, these ranges are extensive are very little sensitive to detect diseases in early stages, which means that some individuals with settings ‘on the edge’ of the normal range could already be in the early stages of a disease.
The theory of triage nutritional
To understand this better, I want to explain the theory of triage nutritional biochemist Bruce Ames of the University of California. The term ‘triage’ comes from the French trier, meaning to sort, and is used in medicine, especially in the emergency department, in order to prioritise the attention when the available resources are overwhelmed by the demand. For example, first served basis to a severely ill patient before one mild, but also before that another very serious that he has no chance of surviving. Bruce Ames adapted this concept to the field of nutrition by proposing that, when the body does not have enough of a nutrient to perform all of its functions, prioritizes the functions vital to the immediate survival at the expense of the secondary, that affect the long-term health and ageing-related diseases, such as cancer.
Let’s look at a couple of examples, the vitamin K and vitamin D.
The main function of vitamin K is to keep a clotting optimal blood, which, in the case of a wound, reduces the risk of dying to bleed to death. In a study with mice, it was shown that when vitamin K is limited, the body prioritizes the coagulation (immediate survival) on secondary functions (long-term health) as protect against bone fragility after the loss of estrogen, the prevention of arterial calcification-related cardiovascular disease), and protection against cancer.
With the vitamin D , something similar happens. Officially, cutting the deficit stood at 30 ng/mL, and from Social Security is not supplemented unless the levels are below that value. Sometimes even in these cases, and when supplemented, it is not done correctly (issue which I have tried in the blog). However, in a meta-analysis that compared the mortality rates for COVID-19 with levels of vitamin D, it is suggested that a theoretical level of mortality zero would be reached levels of approximately 50 ng/mL of vitamin D3 in the blood. This value coincides with another meta-analysis we collected 32 studies conducted between 1966 and 2013, and concluded that the lower mortality rate for all causes of disease lies with vitamin D levels of around 50 ng/mL.
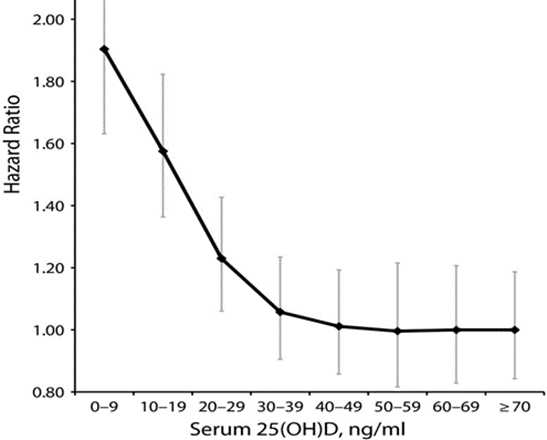
Reasons of risk overall age-adjusted for mortality, in 32 studies
25-hydroxyvitamin D serum in association with mortality for all causes combined: 1966-2013.
Now do you see why it is not the same thing not to have a deficit (within the range of ‘official’) that have something in their optimal point?
Ranges “optimal”
A range of ‘optimal’ for a specific biomarker is one that allows the body to perform all the functions dependent on it, both the few main functions as the many secondary functions, adequately. In addition, it must be at a level that is not excessive or detrimental to the body. This is independent of the average values found in people ‘sound’ of a population.
In summary, there is a deficit according to the rank ‘officer’ only means that the main functions, those vital to the immediate survival, are covered (and that, assuming that the rank is well established). However, when a biomarker is in range ‘optimal’, in addition to ensuring the survival, the body is able to perform secondary functions that are crucial to the health in the medium and long term, which is what really interests me to my clients and readers. After all, we all want to live a little more, but above all, we want to live much better, isn’t it?
It is important to note that correcting a deficit or take a biomarker to your optimal range is almost impossible only with the power supply. Some idealists say that, with a diet perfectly balanced, you can keep everything in its optimal range and that supplementation is unnecessary and just a business. I agree that supplementation is a business, and that there is a lot of marketing, in addition to a lack of regulation that affects the purity of many brands. However, I don’t agree on that supplementation is avoidable if we want to reach our full potential.
In the first place, no one, I repeat, no one wears a power supply with perfectly balanced. And in the second place, no one, I repeat, no one is born with a genetically perfect. We all have a genetic polymorphism that affects the assimilation and metabolism of certain nutrients. The theory is very nice, but anyone with experience in clinical practice knows that all people have something that can improve with proper supplementation.
How can we know the ranges “optimal”. Relationship between biomarker and mortality.
To determine in what range you should be each biomarker, I prefer to build on studies that analyze the relationship between the level of a biomarker and mortality from all causes. These studies investigate what high or low levels of a biomarker is associated with an increased risk of death from any cause, and establish an optimal range in which there is the least probability of death.
These ranges are usually much narrower than the officers, and, in many cases, quite different, as we saw with the vitamin D. Let us consider two other cases related to the cardiovascular risk, which frequently surprise my customers because what they say doesn’t match what they see in their analytical or what your doctor says.
Case 1. cholesterol
I’m not going to extend on to explain what cholesterol is, its beneficial functions, or why we must not seek to have it as low as possible, or to insist that there are no ‘bad guys’ cholesterol (all are good and necessary). Already tried all of this in a previous article. Here, I want to compare the ranks of officers who appear in the leaves of the analytical ranges that indicate the scientific studies on all-cause mortality.
Total cholesterol:
- Range officer: below 200 mg/dL.
- Optimal range: 200-240 mg/dL (study, study, study). As we get older (over 50 years), lower mortality was observed with levels even a little higher.
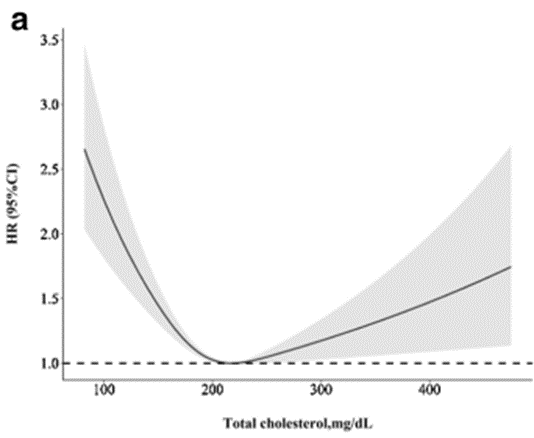
Analysis of splines of all-cause mortality according to levels of total cholesterol. (Adjusted for age, sex, race, level of education, married, smoking, body mass index, systolic blood pressure, estimated glomerular filtration rate, cholesterol of lipoproteins of high density, energy consumption, hypertension, diabetes, antihypertensive drugs, hypoglycemic agents and drugs to reduce lipids)
HDL cholesterol:
- Range officer: More than 40 mg/dL.
- Optimal range: 50-70 mg/dL (study, study, study). In people older than 65 years, the lowest mortality is associated with HDL levels between 70 and 80 mg/dL.
LDL cholesterol:
- Range officer: Less than 116 mg/dL for people with low cardiovascular risk, with lower thresholds for those who have a higher risk.
- Optimal range: 110-150 mg/dL (study, study). In men older than 65 years, the optimal point is about 150 mg/dL, and in women, about 190 mg/dL.
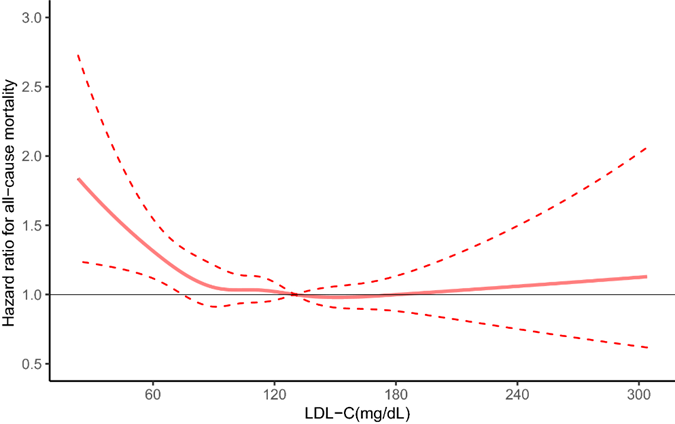
As you can see, cholesterol is not the villain that has been painted. In fact, it is more protective as we age. However, it is still insisting to reduce it more and more, dropping down the ranks officers and prescribing drugs to keep it below those levels.
Try to keep the cholesterol as low as possible to reduce the cardiovascular risk is as forbidding the circulation of cars on the roads to prevent traffic accidents. That something, in this case the cholesterol, is a necessary cause for a disease process (such as the formation of plaque in the arteries) does not mean that it is a sufficient cause nor , even less, the root cause of the disease. If we remove cars from the roads, it is true that there will be no traffic accidents, but the cars themselves, if they are in good condition, are not the ones who cause the accidents, and in addition, the need to.
The crucial question is: what causes the cholesterol to stick to the arteries and form plaques that clog the blood vessels, increasing the risk of heart disease? Cholesterol is good, we need it, protects us, but it must be circular rather than accumulate in the arteries. What we need to address is what causes it to stick, how to maintain a endothelium (the inner lining of the veins and arteries) healthy, increase the size of cholesterol particles (the larger, the less likely it is to be embedded), and prevent the oxidation of cholesterol. How do we accomplish this? By reducing inflammation, homocysteine, glucose, and insulin, and using supplementation with specific vitamins and other nutrients, in addition to adopting healthy habits, such as eating a proper diet, regular exercise, and not smoking.
However, I understand that for many it is easier (and convenient) to resort to a drug that simply reduce cholesterol. I don’t want to be misunderstood: I am not against statins, I think are useful and have their place in certain circumstances, such as in people, by genetics or a lack of healthy habits, not able to keep your cholesterol in ranges suitable and have a context that favors the cholesterol becomes a problem rather than a protection. My criticism is that it abuses its prescribing, administering these drugs to healthy people, and keeping your cholesterol levels below those ranges are optimal, what I think is counterproductive.
I tired to see how people who care, that they eat well, are active and have a context endogenous healthy (low homocysteine levels, APOB, triglycerides, glucose/insulin, C-reactive protein…) are scared because they have seen in their analytical (or your doctor has told you) that you have high cholesterol, with a total of 220 mg/dL, and an LDL cholesterol of 130 mg/dL.
Case 2. homocysteine
Range officer: Less than 15 µmol/L.
optimal Range: Less than 8 µmol/L. (study, study, study).
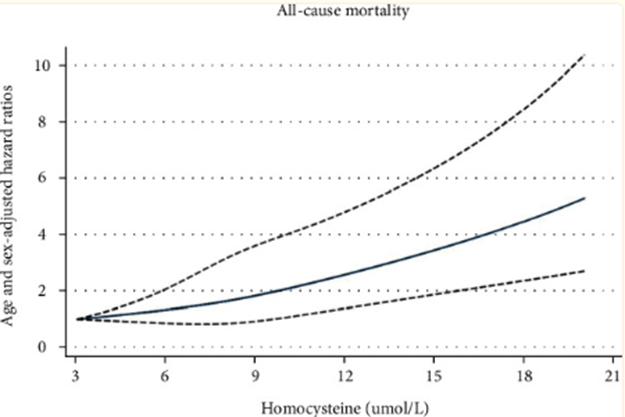
Homocysteine is one of the biomarkers ‘star’ that should be checked in each blood test. Many, many pages of my book Epigenetics nutrition is dedicated to her for the importance in a wide variety of diseases. However, it is often not included in routine analysis, and when measured, it is often interpreted incorrectly. For example, a value of 14 µmol/L is officially considered ‘normal’, but for me, that is unacceptable.
I’m not going to get too deep into this biomarker here, since what I’ll cover in more detail in my next book, but it is crucial to understand that high levels of homocysteine affect very negatively to the whole organism.
To begin with, the homocysteine damages the lining of blood vessels (the endothelium) and promotes inflammatory processes and coagulation. This is precisely what makes cholesterol, which should circulate in the normal way and protect us, is ‘paste’ in the walls of the blood vessels. This process increases the risk of developing cardiovascular diseases such as atherosclerosis (hardening of the arteries), thrombosis (blood clots), heart attacks, and strokes.
In addition, homocysteine elevated increases the risk of developing Alzheimer’s. The blood-brain barrier, which protects the brain from harmful substances in the blood, is mainly composed of endothelium. When this barrier is affected by high levels of homocysteine, it becomes more permeable, allowing the entry of neurotoxins, and other harmful substances in the brain, which contributes to the development of neurodegenerative diseases.
But the homocysteine not only affects the cardiovascular system and the brain, although these consequences by themselves justify to keep it below 8 µmol/L. As I mentioned before, the high homocysteine affects the whole body. If it builds up and is not converted into SAMe (S-adenosylmethionine), a molecule crucial to protect and repair our DNA, our ability to maintain and repair the body is compromised. SAMe is also vital to control which genes are turned on or off (a process known as epigenetics). Therefore, with high homocysteine (and less SAMe), it reduces our ability to protect the DNA, repair damage, and manage the genetic expression of the optimal manner, which leads to accelerated aging, a worse functioning of the body and an increased risk of developing various diseases.
Conclusion:
IS NOT THE SAME AS SOMETHING WITHIN THE RANGE OFFICER
TO BE AT ITS OPTIMUM POINT
I have mentioned only a few examples, but this idea can be applied to almost any biomarker that appears in the analysis of blood. In addition, it is worth noting that the conventional analytical typically ignore biomarkers are crucial for the proper functioning of the body, probably because they are not upgradeable with drugs. Among these are the amino acids in the serum, vitamin B6, selenium, and others that are rarely measured, such as homocysteine, zinc, magnesium, insulin, APOB, and vitamins B9, B12, and D.
Of particular concern is the case of vitamin D. In the rare occasions in which it is measured, its interpretation is often wrong, and when you decide to suplementarla, it is grossly underdosed and using forms of vitamin D less effective for most people, as I already explained in another article.